(Most of) My Overnight Experience:
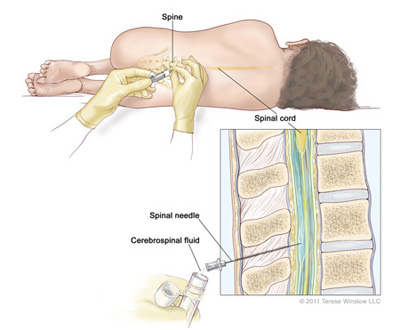
Dr. Limkakeng’s yellow pager rang, and after a brief conversation, he was off! I quickly followed, and we walked past a wall full of medical supplies into a nearby room. An elderly patient had come into the emergency room with cellulitis- a large infection in his jaw. He suffered a seizure for the first time, so Dr. Limkakeng decided to perform a lumbar puncture, or spinal tap, so that the patient’s spinal fluid could be tested for a variety of things such as meningitis. Before performing the procedure, Dr. Limkakeng and a resident explained the pros and cons of a lumbar puncture to the patient’s family members. Agreeing with Dr. Limkakeng’s suggestion, the patient’s wife signed a consent form and the resident got to work. She meticulously sterilized the patient’s back and inserted multiple needles, drawing CSF (cerebrospinal fluid) and containing it in test tubes for the lab. Afterwards, she kindly took the time to explain to me that the CSF would be tested for many things including white blood cell count, which could decipher whether the patient had meningitis.
Like the consent form signed by the first patient’s wife, protocol is very important in the emergency department. Dr. Limkakeng showed me various written guidelines outlining how patient care should be carried out based on certain criteria. For instance, he mentioned that deciding whether a patient should temporarily stay in the observation unit is based on protocol. Treatment of the second patient followed GI protocol, as the patient experienced bleeding. Dr. Limkakeng took into consideration the patient’s history of diverticulitis and diverticulosis, performed an exam, and ordered a CT scan.
The third patient’s treatment involved CT scans as well. She came in with a severe headache, so Dr. Limkakeng and the PA, Melissa discussed the possibility of subarachnoid hemorrhage and a lumbar puncture. Dr. Limkakeng said he was taught that CT scans are not sufficient to indicate SAH, but that there are studies being done on the topic. I found it amazing how even people who are so incredibly knowledgeable in their fields are still in the learning process. The patient’s symptoms quickly completely subsided, so she was discharged later in the night/morning.
That patient didn’t end up needing a consultant, but the next patient required a vascular surgery consultant for her feet. Due to her history of kidney disease and renal failure, combined with hypertension and diabetes, the tissue at the ends of her feet was blackened and fell under the threatened limb protocol. Dr. Limkakeng explained that the immune system attacks dead tissue, so it would likely have to be surgically removed. He also showed me the patient’s x-ray, pointing out the extreme calcification of the blood vessels in her feet. Blood vessels should not be dense like bones, so they should not be visible in x-rays, but hers were so hardened that we could see them quite clearly in the x-ray image.
Another patient across the hall had a similar issue. I asked Dr. Limkakeng if this was common, and he said it is actually rare, so it was simply a coincidence that there were two similar cases in the ED at the same time. Another patient had lower leg issues, though his were less severe. He suffered rashes, fungal infection, bacterial infection, and swelling. A nurse gave him a water pill to begin the healing process, and Dr. Limkakeng gave him further advice.
By 2:37 am, everyone in the Pod B computer area was surprised that there was no one left in the waiting room after a holiday weekend. However, there were still plenty of patients ready to be seen in different rooms. Next was a patient experiencing severe chest pain, and a CT scan was once again very important. The patient was given a contrast liquid to drink so that it would appear white in the CT scan image. Dr. Limkakeng showed me how there was black, showing air, where it should not have been, so thoracic surgery was consulted.
Three of the last patients of the shift showed how much substance use and social stressors impact patients. Dr. Limkakeng talked to me about how substance use greatly affects health directly and indirectly through decision-making. I also observed him navigating patients’ anxiety and stressful events going on in their lives, as it greatly affected their perception of how they felt physically. Overall, my first day observing Dr. Limkakeng in the DUH ED was incredible. The way he treated every single patient with the same utmost respect and kindness was amazing, and I was fascinated by his explanations of EKG’s, CT scans, diseases, how the ED functions, how he decided on his profession, and so much more. Thank you to the doctors, PAs, nurses, and others of the DUH ED for being so welcoming. I cannot wait to learn and experience more on Friday.
Apologies- no photography allowed inside the Emergency Department, and all dates are incorrect on purpose.
Example of a Brain CT Scan
https://en.wikipedia.org/wiki/File:Brain_CT_scan.jpg
Lumbar Puncture
https://curesearch.org/Lumbar-Puncture
Example of Calcification of Arteries
https://www.researchgate.net/figure/Vascular-calcification-of-the-hand-arteries-examined-by-roentgenography-at-a-voltage-of_fig1_266745119